Welcome to Living Proof
The Intracept™ Procedure is supported by strong scientific evidence, including two Level I randomized clinical trials. But the true proof is the living it has restored. You’ll find both kinds of proof here.
Looking for Proof?
Hear from the Ones Living It.
Real Intracept Procedure patients tell their stories of lasting relief from vertebrogenic pain.
What Physicians Are Saying About Intracept
The Data Is Living Proof, Too
The Intracept™ Procedure is supported by unparalleled clinical evidence.
- Four clinical studies that include two Level I randomized controlled trials.
- Study results published in 10 peer-reviewed articles across 7 peer-reviewed journals, with additional systematic reviews and society guidelines on BVN ablation.
Proven Results
- Long-term improvements in pain and function, sustained more than 5 years1
- Sustained decrease in patients using opioids and injections long-term1
- Nearly 80% of patients indicated they would have the procedure again for the same condition1
- Less than 0.2% rate of serious device or procedure-related complications reported.2

Functional improvement.
Statistically sustained improvements in Oswestry Disability Index (ODI – a measure of function) shown 5 years post-procedure.1
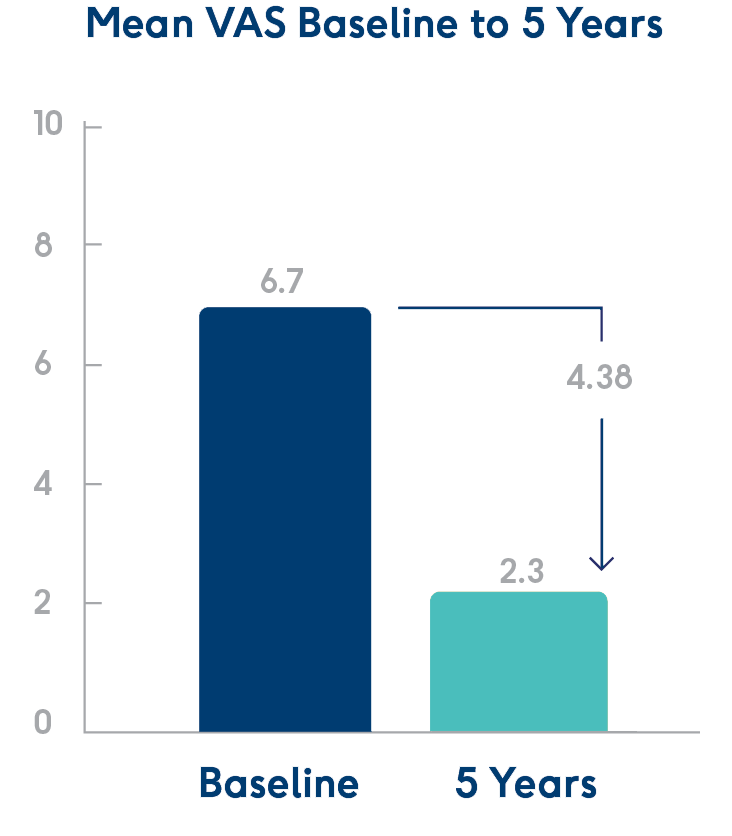
Pain reduction.
Statistically significant reductions in Visual Analog Scale (VAS – a measure of pain) shown 5 years post-procedure.1
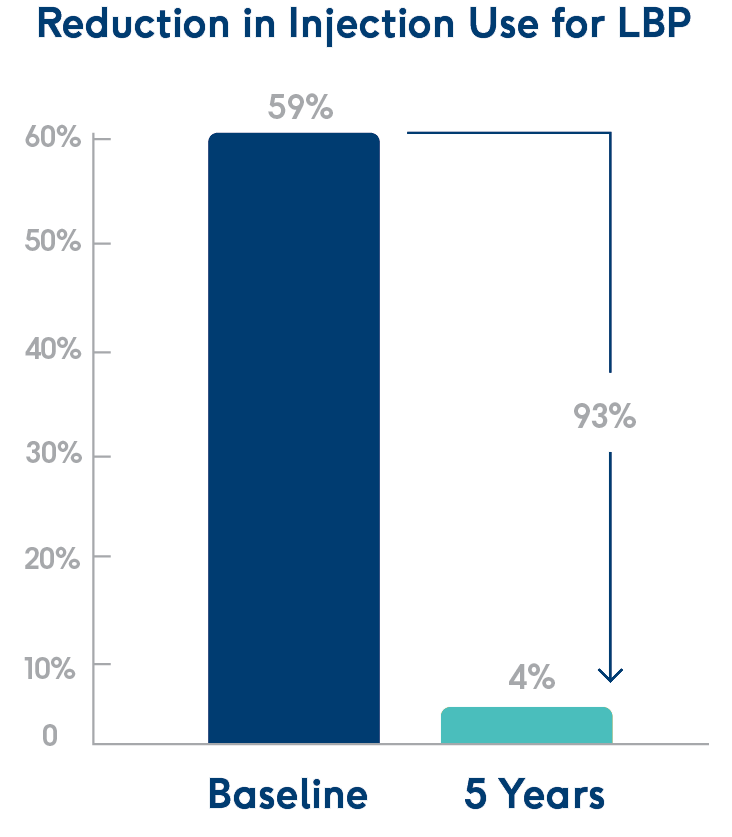
Fewer injections.
At 5 years post-procedure, 93% fewer patients had received injections.1
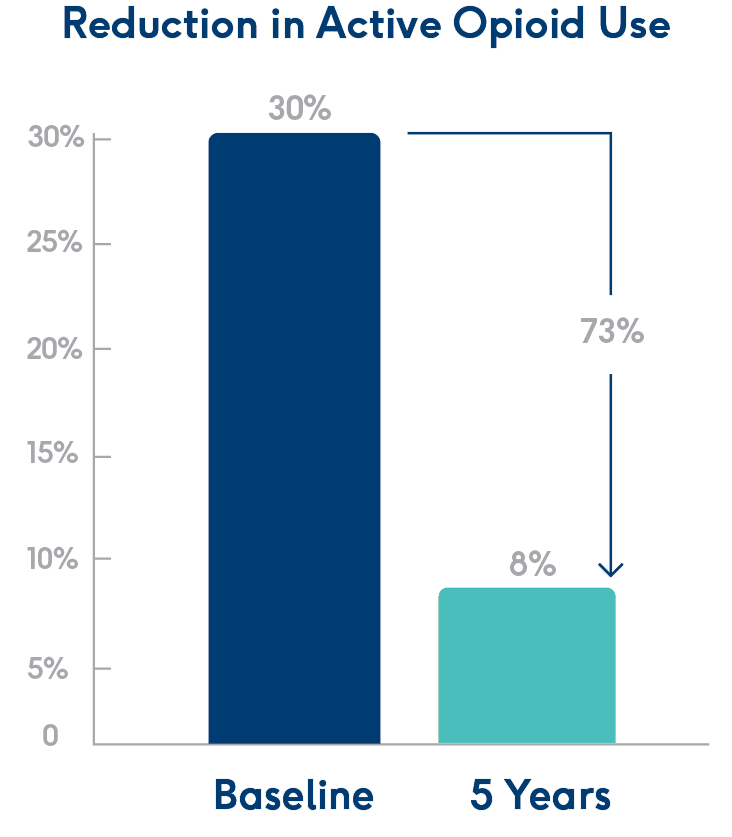
Fewer opioids.
At 5 years post-procedure, 73% fewer patients were actively using opioids.1
As with any surgical procedure, there are risks and considerations associated with the Intracept Procedure. See important safety information below.
Physicians: See Indications, Contraindications, and Risks
Indications for Use: The Intracept™ Intraosseous Nerve Ablation System is intended to be used in conjunction with radiofrequency (RF) generators for the ablation of basivertebral nerves of the L3 through S1 vertebrae for the relief of chronic low back pain of at least six months duration that has not responded to at least six months of conservative care, and is also accompanied by features consistent with Type 1 or Type 2 Modic changes on an MRI such as inflammation, edema, vertebral endplate changes, disruption and fissuring of the endplate, vascularized fibrous tissues within the adjacent marrow, hypointensive signals (Type 1 Modic change), and changes to the vertebral body marrow including replacement of normal bone marrow by fat, and hyperintensive signals (Type 2 Modic change). Contraindications - Use of the Intracept Intraosseous Nerve Ablation System is contraindicated in: Patients with severe cardiac or pulmonary compromise, patients with active implantable pulse generators (e.g. pacemakers, defibrillators), patients where the targeted ablation zone is < 10 mm away from a sensitive structure not intended to be ablated, including the vertebral foramen (spinal canal), patients with active systemic infection or local infection in the area to be treated, patients who are pregnant, and/or skeletally immature patients (generally ≤ 18 years of age). Refer to the Instructions for Use provided with the Intracept Procedure or www.relievant.com/intracept/ for potential adverse effects, warnings, and precautions prior to using this product.
Caution: U.S. Federal law restricts this device to sale by or on the order of a physician.
Copyright © 2025 by Boston Scientific Corporation or its affiliates. All rights reserved.
Patients: See the Indications & Risks Involved
- The Intracept Access Instruments and the Intracept RF Probe are single patient use only. The Introducer Cannula, Diamond Stylet, Bevel Stylet, J-Stylet, Straight Stylet, Drill, and Probe may be used to treat up to a maximum of four (4) vertebrae (L3, L4, L5, S1) on a single patient, while the Curved Cannula may only be used on one (1) vertebra on a single patient.
- As with any surgical instrument, careful attention must be exercised to ensure that excessive force is not placed on the Instruments or Probe. Excessive force can result in product failure.
- Prior to the procedure, CT or MRI imaging must be utilized to help define the desired treatment site and define working anatomical landmarks that can be used for mapping access to the treatment site.
- The device should be manipulated only while under fluoroscopic or CT observation.
- DO NOT use this device in the presence of flammable anesthetics, other flammable gases or objects, near flammable fluids such as skin prepping agents and tinctures, or oxidizing agents. Observe appropriate fire precautions at all times. There is a risk of pooling of flammable solutions under the patient or in body depressions and cavities.
- Fluids pooled in the body depressions and cavities of the patient should be mopped up before RFG is used.
- There is a danger of ignition of endogenous gases (e.g., cotton and gauze saturated with oxygen may be ignited by sparks produced during normal use of the RFG).
- Operator may choose to use smoke-plume extraction apparatus, though the indicated procedure is unlikely to produce noticeable smoke
- The Probe is for use WITHOUT a neutral electrode (ie., a grounding pad).
- Discontinue use if inaccurate, erratic or sluggish temperature readings are observed. Use of damaged equipment may cause patient injury.
- Prior to operation, visually inspect the Probe and RF for physical damage, obvious cracks in insulation or loose parts.
- During power delivery, the cable should not come in direct contact with the patient's skin or other patient leads.
- Safety and effectiveness in patients with conditions that are associated with poor bone quality such as osteoporosis have not been established.
CONTRAINDICATIONS
Use of the Intracept Intraosseous Nerve Ablation System is contraindicated in:
- Patients with severe cardiac or pulmonary compromise
- Patients with active implantable pulse generators (e.g. pacemakers, defibrillators)
- Patients where the targeted ablation zone is < 10 mm away from a sensitive structure not intended to be ablated, including the vertebral foramen (spinal canal)
- Patients with active systemic infection or local infection in the area to be treated
- Patients who are pregnant
- Skeletally immature patients (generally ≤ 18 years of age)
WARNINGS
- Do not use if package is opened or damaged as product integrity and/or sterility may be compromised.
- Do not use after the expiration date has passed as product integrity and/or sterility may be compromised.
- Do not re-sterilize or reuse. Re-sterilization or reuse may result in cross contamination, patient infection, or device malfunction.
- Reconditioning, refurbishing, repair or modification of the device to enable further use is prohibited.
- Do not use this product if you have not been properly trained in its use. Physicians using the device should be familiar with the physiology and pathology of the selected anatomy to be treated and be trained in the performance of the chosen surgical technique. Improper surgical use and technique may lead to suboptimal clinical outcomes.
- Read and understand the Instructions For Use ("IFU*) completely prior to use.
- The Intracept System must be used with the Relievant Medsystems RF Generator in order to provide the required treatment parameters.
- Failure of the RFG could result in an unintended increase of output power to the Probe.
- The Intracept RF Probe may interfere and adversely influence the operation of other electronic equipment.
- Fischgrund J, Rhyne A, Macadaeg K, et al. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2020;29(8):1925-34. doi.org/10.1007/s00586-020-06448-x
- Data on file.
NM-2011812-AA